New Pharmacovigilance
Initiative
UM and Humana Launch Effort
to Research Adverse Drug Events
![]() he
Miller School of Medicine and health insurer Humana, already partners
in a health services research center, announced a groundbreaking Pharmacovigilance
Initiative, a prescription drug usage tracking and analysis program that
will mine information from Humana’s 11 million-member database.
he
Miller School of Medicine and health insurer Humana, already partners
in a health services research center, announced a groundbreaking Pharmacovigilance
Initiative, a prescription drug usage tracking and analysis program that
will mine information from Humana’s 11 million-member database.
At a time when news reports relay troubles with drugs such as Avandia and Vioxx after they have been tested and placed on the market, UM doctors and Humana executives said the new program will provide timely, real-world analysis of how patients use certain medications, document emerging patterns of adverse impacts and, as appropriate, issue results to physicians and the Food and Drug Administration.
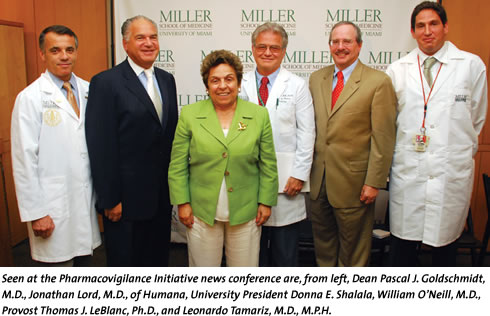
Combining the expertise of UM with data from Humana makes “a very unique program. Through our partnership we’re going to focus on prescription drug safety,” University President Donna E. Shalala said at the August 22 news conference.
Describing the initiative as extremely valuable for users of prescription drugs, Miller School Dean Pascal J. Goldschmidt, M.D., said it is “the right thing to do, at the right time” to help fill a gap in the cycle that takes new drugs from development to the marketplace.
The program was hailed by other participants in the news conference, including Jonathan Lord, M.D., senior vice president and chief innovation officer at Humana, and from UM, William O’Neill, M.D., executive dean for clinical affairs, and assistant professors Leonardo Tamariz, M.D., M.P.H., and Hermes J. Florez, M.D., M.P.H., researchers at the UM-Humana Health Services Research Center.
The Pharmacovigilance Initiative will operate out of the Health Services Research Center, a public-private partnership established in 2005 to focus on health services and health behavior research.
The Miller School-based center undertakes various scientific studies such as one that looked at 7,091 Humana patients who had stents implanted between January 2003 and June 2005. It found that bare-metal stents were associated with a higher risk of myocardial infarction than drug-eluting stents, but the risk might be mediated because patients on bare-metal stents used the antiplatelet drug clopidogrel less often and for shorter periods of time than drug eluting-stent patients.